Our understanding of what matters for helping people and communities achieve better health and how best to do it has evolved dramatically over the past decade. Increased availability of large integrated data sets and sophisticated analytics have helped to narrow some gaps in care and improve certain outcomes. Widespread acceptance that our physical health is greatly impacted by our mental health and social determinants of health (SDOH)—the conditions and circumstances in which we live—has led to models of care that now integrate important behavioral health and community services. Healthcare technologies, such as video visits, are making healthcare more accessible and affordable without impacting care quality.
While all these represent important progress, the U.S. still faces complex problems that challenge our shared goal of improving health for all. Stark disparities in health outcomes and care access persist for underrepresented population groups, economic uncertainties and a continued rise in healthcare costs are impacting healthcare affordability for working Americans, and an aging population affected by greater and costlier disease burdens is driving demand for more healthcare services—to name a few.
Research, evaluation, and knowledge dissemination are and will continue to be key activities for overcoming healthcare challenges while sustaining important progress. Historically, though, these activities have not occurred in ways that have helped healthcare systems respond most effectively in a rapidly evolving healthcare landscape. Today’s healthcare systems need the right expertise, approaches, and collaborations embedded within the organization to efficiently generate and translate new knowledge into healthcare services and practices that are beneficial and meaningful to those that use them.
--------
The UPMC Center for High-Value Health Care’s Approach to Supporting Progress in Healthcare
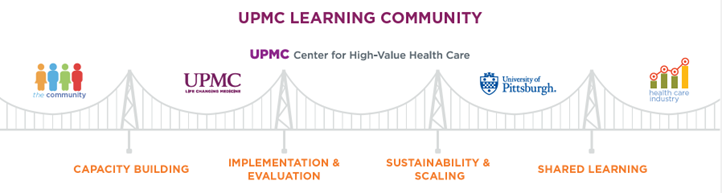
Since 2011, the UPMC Center for High-Value Health Care (Center) has used patient-centered outcomes research, comparative effectiveness studies, program evaluations, implementation science, and patient and community engagement activities to understand how new healthcare delivery and payment models impact health and cost outcomes within UPMC and beyond. As an integral component of UPMC’s Learning Community [Figure 1], the Center conducts these activities by fostering collaborations with researchers, providers, patients, caregivers, policy experts, and advocates across UPMC, the community, and the healthcare field at large. By engaging a wide range of stakeholders in research, evaluation, and knowledge dissemination activities, the Center helps to ensure that their experiences and perspectives shape and inform the important questions we seek to answer and actionable evidence that is translated into practice.
Figure 1: UPMC’s Learning Community Framework


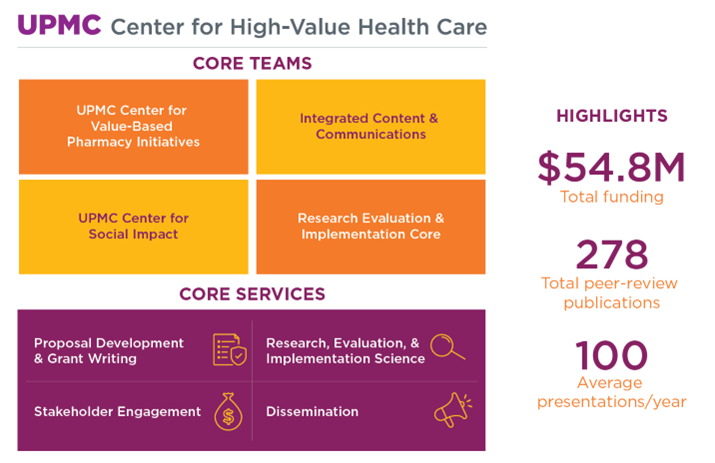
The Center [Figure 2] is a nonprofit entity housed within the UPMC Insurance Services Division and includes the Center for Social Impact and Center for Value-Based Pharmacy Initiatives. Many Center activities are supported through grants and contracts and conducted in collaboration with community organizations and government agencies. We work closely with teams within UPMC and other network providers to improve the quality of services offered to UPMC patients and members. Since 2011, our team has been awarded over $50 million in external funding and has supported more than 55 projects within UPMC.
In addition to catalyzing and testing innovation, we disseminate findings through peer-review publications, presentations at academic and trade/industry conferences, and other stakeholder engagement activities. Our quarterly Innovations in Health Care webinars showcase impactful work and explore the nuances of healthcare issues with topical experts. Through our Integrated Content and Communications Strategy, we further translate and disseminate thought leadership insights and findings to member, provider, government, and general media stakeholder audiences, as well.
Figure 2: The Center for High-Value Health Care’s Structure and Highlights


Who staffs the Center and what do they do?
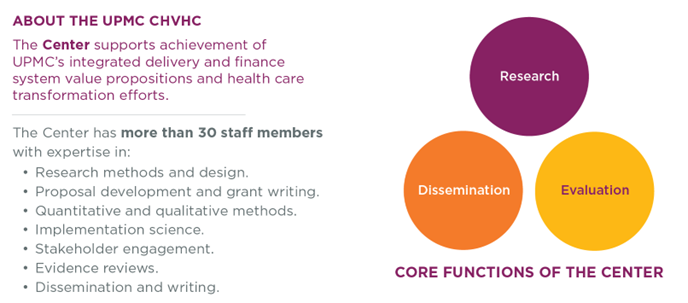
The Center comprises health services researchers, methodologists, analysts, and research administrators who develop and execute comprehensive evaluation plans and apply quantitative and qualitative research methods in real-world contexts with the goal of producing new, relevant, and trusted knowledge that is useful toward achievement of UPMC business goals and objectives [Figure 3].
Figure 3: UPMC Center for High-Value Health Care Staff and Their Expertise


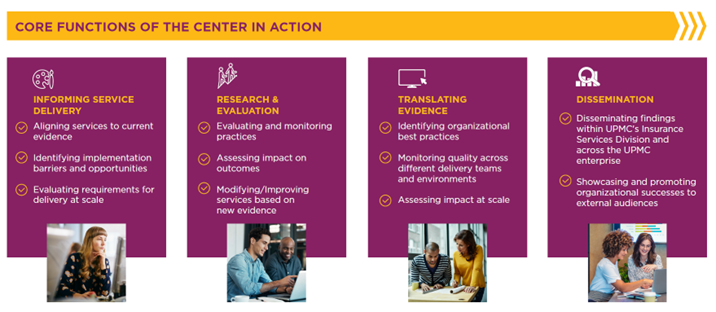
How does Center staff conduct research and evaluation?
Center staff engage in a continuum of health services research and evaluation activity [Figure 4]. We design, implement, and evaluate research and pilot programs. We work with our stakeholders to scale successful research findings and pilot programs across the learning community. In all stages of research and evaluation, we share learning throughout UPMC and the community it serves as well as across the healthcare industry.
Figure 4: The Health Services Research and Evaluation Continuum


How does the Center’s health services research, evaluation, and stakeholder engagement work address healthcare challenges?
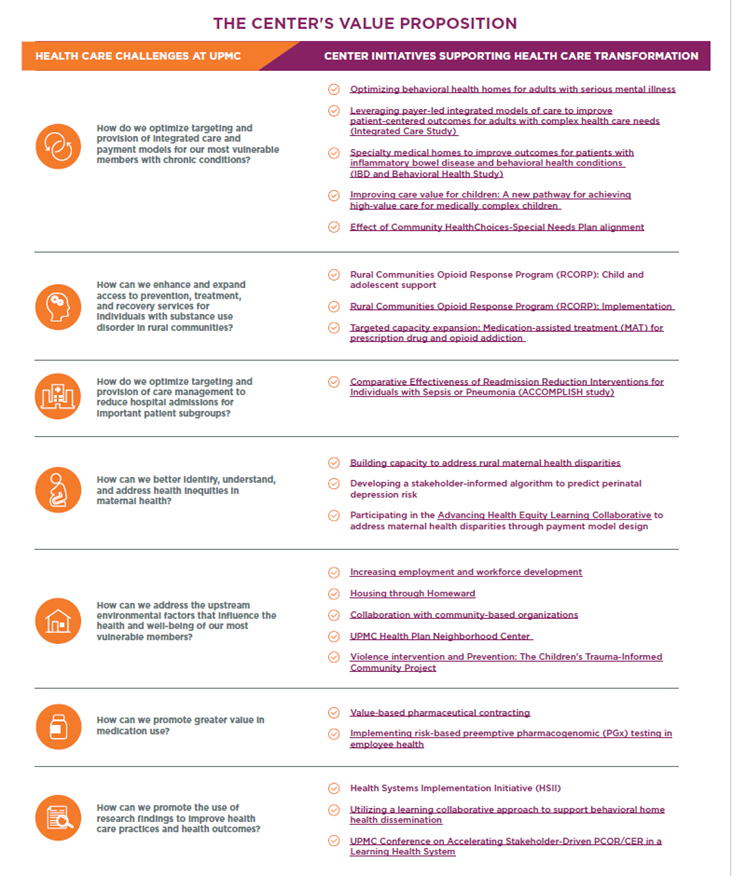
The Center’s research, evaluation, and stakeholder engagement portfolio reflects the challenges and priorities deemed most important by UPMC, its collaborators, and the greater healthcare industry [Figure 5].
Figure 5: Healthcare Challenges and the Key Research, Evaluation, and Stakeholder Engagement Activities to Address Them


Want to learn more about the UPMC Center for High-Value Health Care? Visit Our Work to learn more about our current and past initiatives, including our efforts in the areas of Value-based Pharmacy Initiatives and Social Impact. Look up our 250+ publications within our Resource Library. Connect with us.